Greg Gies
For 20 years in the software industry, Greg Gies has been helping businesses, government agencies and healthcare organizations achieve their goals and carry out their missions by making better use of information and automating business processes. Greg has held positions in sales, product management and marketing and holds an MBA from Babson College. He works and lives with his wife and three boys in the Boston area. You can read more of Greg’s blog posts here and connect with Greg on LinkedIn.
Posted by
Greg Gies
on Jul 26, 2016 8:00:00 AM
The U.S. Department of Health and Human Services defines Quality Improvement (QI) as systematic and continuous actions that lead to measurable improvement in health care services and the health status of targeted patient groups.
While procedures and systems are necessary to ensure continuity, equally important is the measurement of actions and patient health status, which require data not only to establish a baseline but also to continuously track, monitor and measure progress toward QI goals.
Read More
Posted by
Greg Gies
on Apr 30, 2016 10:10:00 AM
Spend more time finding a cure and less time finding and redacting PHI.
Preparing patient records for research analysis is a painstakingly laborious process. De-identifying records is the main culprit. Manual point-and-click redaction tools are no match for large-scale jobs involving complex patient records.
Read More
Posted by
Greg Gies
on Apr 30, 2016 9:48:00 AM
Your incomplete data set doesn’t tell you the full story.
 A population health management program without the ability to analyze a complete set of clinical data is like reading a book with missing pages. You’re left with only your imagination to fill in important details.
A population health management program without the ability to analyze a complete set of clinical data is like reading a book with missing pages. You’re left with only your imagination to fill in important details.
Read More
Posted by
Greg Gies
on Apr 30, 2016 9:31:00 AM
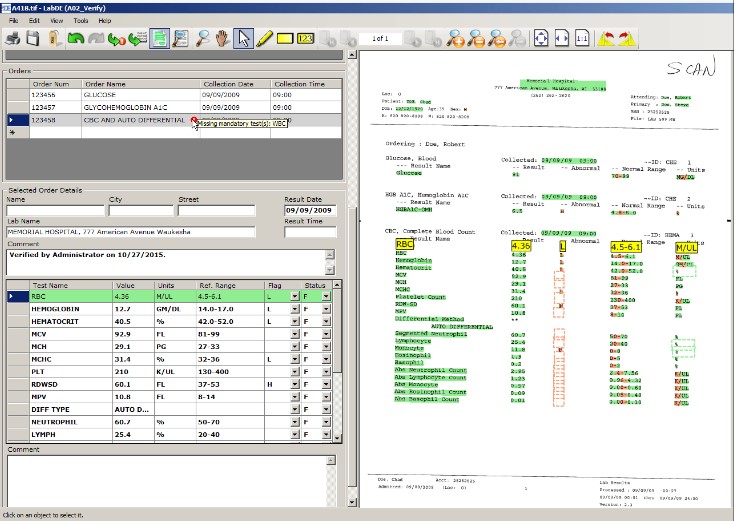
Clinical labs should be tests for your patients, not a test of your patience.
Delivering high quality care in a timely manner is the best way to ensure patient safety and satisfaction. Clinical labs are often a critical step on the path to diagnosis and treatment. Test results from outside labs are often delayed or hard to find amid a sea of PDF files in the EHR, or worse, in a pile of paper faxes.
Read More
Posted by
Greg Gies
on Apr 30, 2016 9:20:00 AM
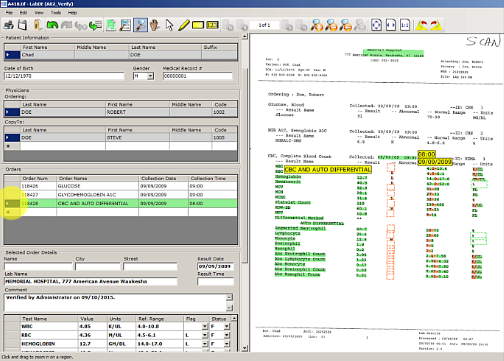
No interface? No problem. Automatically capture send-out test results into your LIS.
Unfortunately, setting up lab interfaces to every reference lab isn’t an option. This is especially true for low volume, high value esoteric labs.
Consequently, communications of test results are delayed while test data is keyed in. Manually keying test results in the LIS is slow, error-prone and, when done correctly with redundant data entry, imposes a high opportunity cost.
Read More
Posted by
Greg Gies
on Apr 30, 2016 6:00:00 AM
Only meeting the minimum MU2 core measure for labs compromises clinical decisions costing $317,178 per bed each year.
Meaningful Use Stage II core measure for lab results requires that lab values are captured in structured EHR data fields for only 55% of results. That means as many as 45% of decisions informed by test results that aren’t easily accessible or trendabale -- driving up the cost of care and compromising care quality.
Read More
Posted by
Greg Gies
on Feb 11, 2016 9:43:42 AM
Despite massive adoption of electronic medical records over the past several years, the promise of easy and nearly effortless chart abstraction from electronic medical records enabled by an interconnected web of interoperable EMRs sharing standardized data has yet to be fully realized. You need to look no further than the media tab to see the evidence that we have yet to arrive at this utopian future.
Read More
Posted by
Greg Gies
on Feb 2, 2016 10:54:47 AM
Clinical data abstraction is often one of the last steps in the patient care information workflow. Typically it's performed for the sole purpose of submitting data to compliance or quality improvement measurement programs.
What if you were able to perform data abstraction immediately upon receiving medical records from outside providers (labs, diagnostic test centers, pathologists, etc...) and capture the data in the designated, structured EMR data fields before patient care begins?
Would having that information in discrete fields in the EMR from the very beginning of the patient's journey be helpful and might it have a positive effect upon the overall quality of care?
Read More
Posted by
Greg Gies
on Feb 1, 2016 12:18:17 PM
Recently, Andy Slavitt, the CMS acting administrator, announced that CMS will likely end the Meaningful Use program this year.
Does that mean that the hopes of an internetworked healthcare system that’s able to seamlessly share health information are completely dashed before interoperability truly got off the ground?
The answer to that question remains to be seen.
Read More
Posted by
Greg Gies
on Jan 19, 2016 7:00:00 AM
Critical results reporting or reporting lab results for priority patients from non-interfaced sources is no easy task. A delay in reporting can yield an unfortunate outcome for a patient whose condition is deteriorating. This is especially true for specialty departments that provide continued care for patients from far-flung locales, such as the transplant program. One transplant department receives thousands of these reports over a single patient's lifetime, and often hundreds of these documents for its patient population each day by fax.
Until now, critical results management solutions have ignored the chore of sifting through these unstructured documents to report results to the care team. Consequently, handling these results has stubbornly remained a manual, cumbersome and error-prone process.
Extract Systems has developed a solution that not only automatically identifies lab reports for priority patients upon arrival. It also extracts and posts the data into the patient's EMR — a task that typically falls on the shoulders of thinly stretched staff.
Read More

 A population health management program without the ability to analyze a complete set of clinical data is like reading a book with missing pages. You’re left with only your imagination to fill in important details.
A population health management program without the ability to analyze a complete set of clinical data is like reading a book with missing pages. You’re left with only your imagination to fill in important details.